Everything You Need To Know About Lupus
It Causes Long-Term Inflammation
Lupus – officially known as systemic lupus erythematosus (SLE) – is a long-term condition that can cause inflammation in any part of the body. In people with lupus, the immune system produces far too many antibodies, which circulate around the bloodstream and attack healthy tissues.
In around half of systemic lupus cases, a major organ or tissue in the body, such as the heart, lungs, kidneys, skin or brain will be affected. These organs can be damaged in an irreversible way.
It Mainly Affects Women
Lupus is estimated to affect over five million people worldwide, and 90% of those are women. It mostly strikes women of childbearing age, with the majority of people developing the disease between ages of 15 and 55. It’s also more common black and Asian women.
However, men, young teenagers and children can develop lupus, too. The average age of diagnosis for paediatric lupus is just over 12 years old, and girls are affected four times more frequently than boys.
It Can Be Triggered By Various Things
The main trigger of lupus – and the reason it affects so many more women than men – is hormonal activity and change. Childbirth, the menopause and puberty can often trigger the disease.
Viral infections, strong medication, sunlight, trauma and environmental factors are thought contribute in some way too. Any two or more of these triggers can also combine to set off the illness.
While doctors currently don’t know exactly what causes lupus, studies have shown that genes play a role – certain genes can make a person predisposed to developing lupus and affect the severity of their symptoms.
It’s Difficult To Diagnose
Lupus can produce a large number of symptoms – a lot of which can be similar to other conditions, so GPs often fail to recognise it. The two major symptoms are joint and muscle pain and an extreme tiredness that won't go away, no matter how much you rest. Rashes, depression, anaemia, feverishness, headaches, hair loss and mouth ulcers may all be part of the pattern of lupus too.
While the two major symptoms are invariably present, people with lupus can differ greatly in their symptoms and how the illness affects them – life-threatening for a few, and very mild for others. People can also find their symptoms wax and wane, with periods of no symptoms followed by a flare-up.
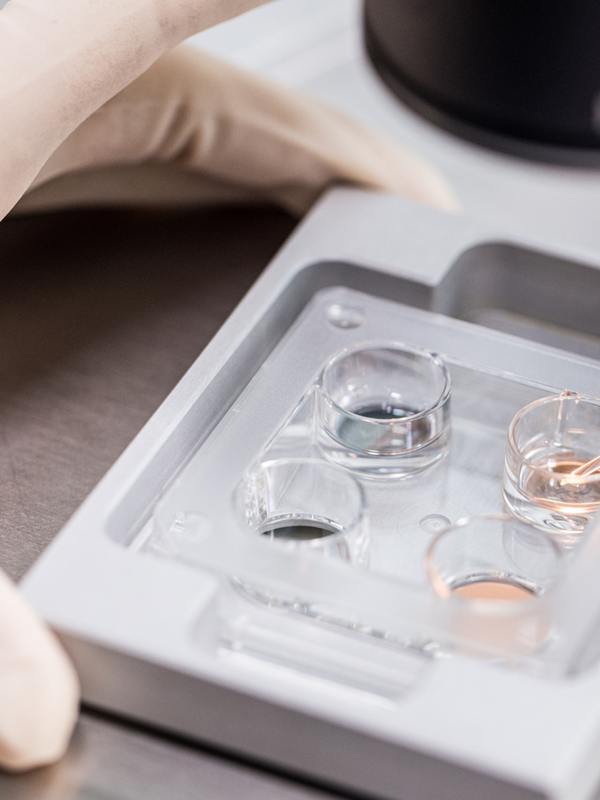
To diagnose lupus, your GP will need to refer you for a blood test. High levels of a specific type of antibody, combined with typical symptoms, can mean lupus is likely. You may then be referred for X-rays and scans of your heart, kidneys and other organs if your doctor thinks they might be affected.
According to the NHS, you should see a GP if you have:
- Joint pain and stiffness
- Extreme fatigue
- Skin rashes – often over the nose and cheeks
- Unexplained weight loss
- Swollen glands
- Sensitivity to light (causing rashes on uncovered skin)
- Poor circulation in fingers and toes (Raynaud's)
It’s Incurable, But Treatable
There is no cure for lupus at present, but the disease is better managed if diagnosed and treated early. Once diagnosed, you'll be advised to have regular checks and tests, including blood tests to check for anaemia and urine tests to check for kidney problems, which lupus can cause.
Lupus is generally treated using antimalarials (such as hydroxychloroquine) and non-steroidal anti-inflammatory drugs (like ibuprofen). Steroids and immunosuppressants are also used in more severe cases and can be life-saving. And although medicines are important in controlling lupus, the NHS advises people make the below lifestyle changes to help manage their symptoms and reduce the risk of the disease progressing:
- Eating a healthy, balanced diet
- Staying active, even during flare-ups
- Getting lots of rest
- Trying relaxation techniques to manage stress
- Avoiding sitting in direct sunlight or fluorescent light
- Using a high factor sunscreen (SPF50+)
- Wearing a hat in the sun
- Not smoking
For more support, advice and information about lupus, visit LupusUK.org.uk
DISCLAIMER: We endeavour to always credit the correct original source of every image we use. If you think a credit may be incorrect, please contact us at info@sheerluxe.com.