Artificial Ovaries Could Help Women Become Mothers After Cancer
Researchers from Copenhagen’s Rigshospitalet, one of the leading fertility centres in Europe, say they have demonstrated the world’s first working ‘bio-engineered’ human ovary in early animal trials. During the research project, their lab-made ovary was able to keep eggs alive for weeks at a time, which has further raised hope for use in reproductively-challenged humans in the future.
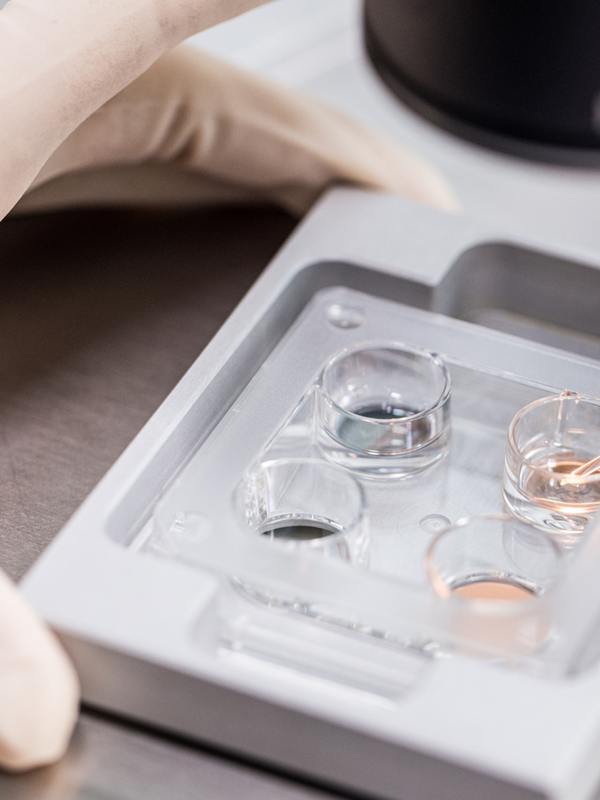
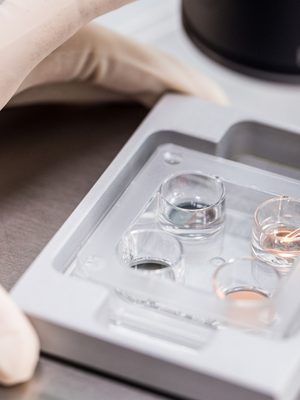
To create one of these ovaries, chemicals were used to strip ovarian tissues of DNA and other features, including any faulty cancer cells. This left an empty tissue ‘scaffold’ which is made of mostly collagen (the protein that gives skin its strength). Immature egg cells were planted into this scaffold, and researcher Susanne Pors and her team at Rigshospitalet were able to demonstrate the eggs were able to survive and reintegrate. In theory, the eggs would then begin to mature and release each month in line with a woman’s menstrual cycle.
“This is the first time that isolated human follicles have survived in a decellularised human scaffold,” said Pors, who presented her team’s findings at the European Society of Human Reproduction and Embryology (ESHRE) annual meeting in Barcelona earlier this month. During her presentation, Pors detailed how the team implanted an artificial ovary holding 20 human follicles into a mouse and found that a quarter of them survived for at least three weeks. During that time, blood vessels began to grow around the ovary, which was kept well-nourished inside the creature.
“This is the first proof that we can actually support these egg cells. It’s an important step along the road,” Pors told the Guardian, adding that there would need to be a lot more research before they could think about human implementation. “It will be many years before we can put this into a woman,” she said, revealing it will likely be another five to ten years before artificial ovaries are fit for human trials.
Nick Macklon, Medical Director at London Women’s Clinic, concurred with Pors, stating that her team’s findings were an “exciting development”, but the project still needs further advancement: “This is early days for the work but it’s a very interesting proof of concept.”
Artificial ovaries would help women with conditions such as multiple sclerosis, the blood disorder beta thalassaemia, women thrown into an early menopause and those diagnosed with cancer. In the case of the latter, some women can already have all or part of an ovary removed and frozen before treatment, for the purpose of re-transplanting it back in after surgery. But this can be risky – the reintroduction of the ovary runs the risk of implanting dangerous cancerous cells that could be hidden in the preserved tissue.
In this sense, an artificial ovary would reduce a large element of risk. It could even be an improvement on other fertility techniques such as IVF, as more potential eggs could be preserved and developed more naturally.
Recently, medical advances related to the fertility of women has progressed significantly. In June, it was revealed doctors will soon be able to perform womb transplants on women in the UK. The procedure will use live donors – which means the patient receiving the womb will likely have been donated it from a family relation, such as her mother or sister. The gestation period for the baby will be slightly less – around 35-37 weeks – and would be delivered via caesarean section. This also equates to a shorter surgery time and reduced health risks, which can include clot formation, deep vein thrombosis and damage to pelvic organs.
Many are taking the news as a positive step in the right direction for women who struggle to conceive. With a womb transplant, women who were previously unable to experience pregnancy and childbirth can do so if they wish. The same would be true for women with an artificial artery – it gives women the chance to experience childbirth in a way that they had previously been denied.
DISCLAIMER: We endeavour to always credit the correct original source of every image we use. If you think a credit may be incorrect, please contact us at info@sheerluxe.com.