Are You Going Through The Perimenopause?
What exactly is the perimenopause?
“While the menopause officially starts one year after your last period, the perimenopause is the period of time leading up to that. The menopausal symptoms people refer to are often actually perimenopausal symptoms. Levels of the female hormones oestrogen and progesterone are fluctuating as our periods stop and eventually drop to very low levels after the menopause. Levels of testosterone, which is classically thought of as a male hormone, are also dropping, which contributes to the majority of symptoms and physiological changes.” – Dr Anita Mitra, consultant clinical oncologist, aka the Gynae Geek
When does it happen?
“The perimenopause doesn’t just happen to ‘old’ women. The menopause (so 12 months after your last period) occurs on average at the age of 51. However, many women experience perimenopause in their 30s and 40s, some even in their 20s. Some women experience the perimenopause around the same time their mother did, so this can be an indicator. There are also many other factors that can lead to a surgical menopause – these include cancer and a hysterectomy. Some radiotherapy treatments can also induce an early menopause.” – Victoria Howell, registered nurse, coach and women’s health specialist
“The average age of the perimenopause is 47. Your mother’s age can be a bit of a guide but I don’t hold too much to it. Women nowadays have a different lifestyle to their mothers – work, partying, different relationship statuses, drinking and smoking, and these can all affect your age of menopause. For example, if you are a smoker, you are more likely to go through the menopause 2.8 years earlier.” – Dr Shahzadi Harper, The Menopause Doctor and founder of The Harper Clinic
How long does it last?
“It varies significantly from woman to woman. The average duration of the perimenopause is four years, but it can range from a few months to ten years.” – Anita
What are the symptoms?
“There is a huge array of symptoms, and not all women will get all of them. These can include hot flushes, night sweats, headaches, lack of energy, painful joints, insomnia, poor concentration, palpitations, irritability, loss of libido, restless legs, thinning hair, digestive issues and increased allergies. Anxiety is one less obvious symptom that is often not recognised as being linked to the perimenopause – perhaps you have never been an anxious person and are suddenly experiencing anxious thoughts before your period, or have previously suffered with anxiety and find it hits you on a whole new level prior to your period. Crying spells are also common, especially about things that seem irrational. Low mood, depression and mood swings are also common – these tend to be similar to premenstrual symptoms but may feel more intense and last longer. Brain fog can also occur – this is due to changing levels of oestrogen.” – Victoria
“There’s also the less sexy stuff that women are often shy to talk about – vaginal dryness and irritation, urine leakage and hairs in places that were previously fuzz-free.” – Anita
Are you still fertile in perimenopause?
“Yes. During the perimenopause women still ovulate, and the uterus may well have the right environment for conception to take place. If you are not planning on a pregnancy then you still need to use contraception. Women have been known to become pregnant post-menopause, which is why guidelines recommend contraception is used up to two years following your last period.” – Victoria
What treatment options are available?
“The perimenopause is an excellent time to start topping up oestrogen because of the benefits to long-term health. Hormone replacement therapy (HRT) is the first recommendation – this tops up and/or replaces the oestrogen in our bodies, largely eradicating symptoms, helping women to feel better about themselves. HRT can also protect bones from osteoporosis, and emerging evidence suggests HRT can reduce the risk of dementia and cognitive decline. If you are considering HRT, try and see a GP who’s trained in the menopause or a private practitioner. Sadly, many GPs have no training in the menopause and women have been misdiagnosed and given antidepressants or other incorrect advice as a result. The best forms of HRT come in patch form, gel or spray.” – Victoria
Is HRT safe?
“No medical treatment is without its risks. An assessment of the risks versus the benefits should always be undertaken when starting any medication. The main risks are:
BLOOD CLOTS: There is a slightly higher risk with tablets compared to transdermal HRT and in women with a BMI over 30. Therefore, doctors avoid prescribing tablets to women with a higher BMI in favour of transdermal options.
STROKE: Again, there is a slightly higher risk with tablets, especially for those over 60. Below this age, the risk is very negligible.
BREAST CANCER: HRT that contains oestrogen and progesterone has been linked with a slight increase in breast cancer. The theory is that the medication promotes the growth of a small number of cancer cells already present, rather than actually causing the disease.” – Anita
Are there any alternatives?
“Sage, black cohosh, red clover and acupuncture can all help with hot flushes; ginkgo biloba and ashwagandha can help with a low libido; vitamin B and St John’s Wort are all good for a low mood; and calcium, vitamin D, omega-3 and turmeric can all ease joint pain. Studies also suggest CBD and magnesium can aid anxiety and sleep problems.” – Shahzadi
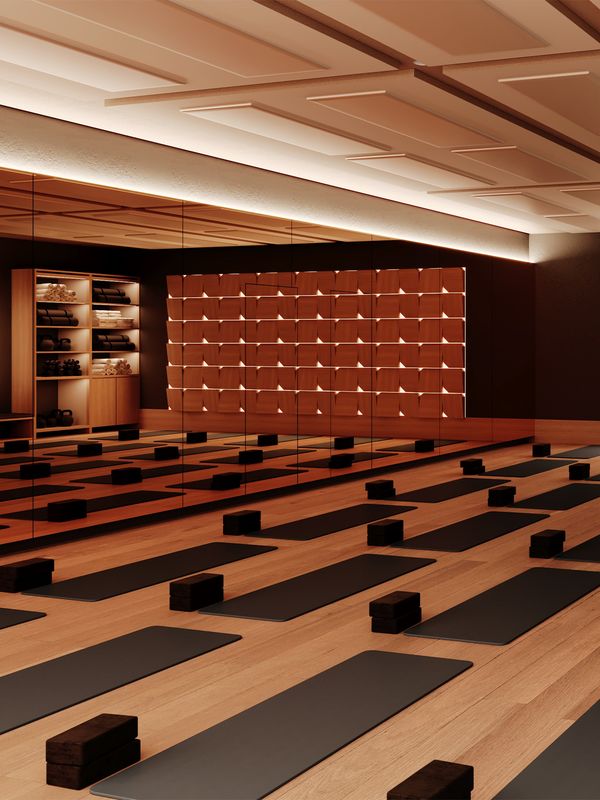
“There are many complementary therapies that can be used to support women, such as yoga, mindfulness, acupuncture and CBT. However, research into the efficacy and safety of these is currently lacking.” – Victoria
Are there any dietary changes that can ease symptoms?
“Consider eating more foods that are rich in phytoestrogens (plant-based sources of natural oestrogen) such as oats, lentils, flaxseeds, soybeans, broccoli and wheat bran. Isoflavone-rich foods, such as nuts and chickpeas, can also help. Eating fresh food over processed food will also help, so try to cut down on foods that have hidden salt and sugar. Also try to drink two litres of water daily. When it comes to lifestyle, quitting smoking and cutting back on alcohol will reduce symptoms, especially hot flushes. Think about keeping a food diary, which can be a useful visual tool to identify if certain foods trigger certain moods or symptoms.” – Victoria
“Your metabolic rate slows down in your 40’s, so women need 200 fewer calories per day and should remember to include a protein source in each meal, which will keep you filler for longer and help maintain muscle. Muscle loss is common during perimenopause – good sources include eggs, almonds, chicken, turkey, quinoa, lentils and Greek yoghurt. A supplement can also help for mild perimenopausal symptoms – Promensil UK, Menopace and Femarelle are all good brands.” – Shahzadi
Is there anything younger women can do to minimise potential problems later on?
“The earlier you get your hormones in check, the better. Your hormones naturally go haywire during the perimenopause, so whilst it’s not too late to do anything about it, if you’ve got good ‘hormone hygiene’ before it happens then you’re likely to fare better.” – Anita
“Be prepared, but don’t be scared. Menopause is a natural process and could happen sooner than you expect. Around 5% of women will have a naturally early menopause so if you’re interested in having children, don’t leave it too late. Also, try to manage your weight as you get older – this is good for your long-term heart health and also a reduced risk of breast cancer. Don’t forget to do your pelvic floor exercises, either. After the menopause, the decline in oestrogen levels makes women more likely to suffer from urinary incontinence as well as vaginal dryness and atrophy, so it’s worth getting your pelvic floor in shape. The earlier in life you tackle the lifestyle factors – smoking, drinking, exercise and eating well – the better prepared you’ll be.” – Shahzadi
For more information visit GynaeGeek.com and TheNorfolkCoachingCompany.co.uk. To book an appointment with Dr Shahzadi Harper visit TheHarperClinic.com
*Features published by SheerLuxe are not intended to treat, diagnose, cure or prevent any disease. Always seek the advice of your GP or another qualified healthcare provider for any questions you have regarding a medical condition, and before undertaking any diet, exercise or other health-related programmes.
DISCLAIMER: We endeavour to always credit the correct original source of every image we use. If you think a credit may be incorrect, please contact us at info@sheerluxe.com.